Vascular diseases
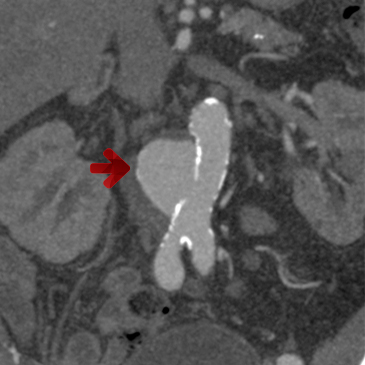
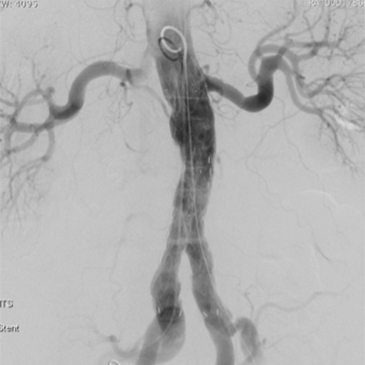
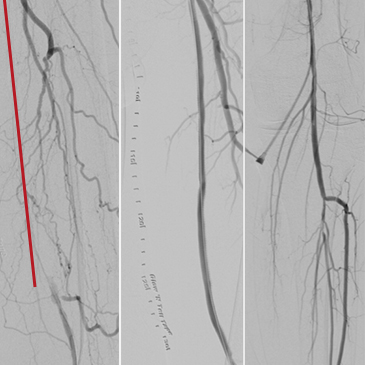
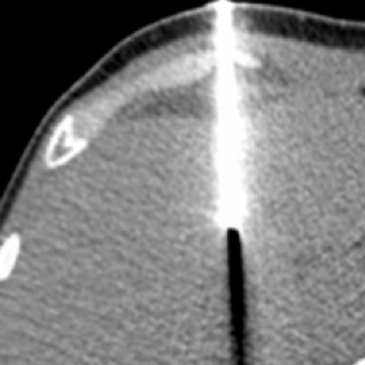
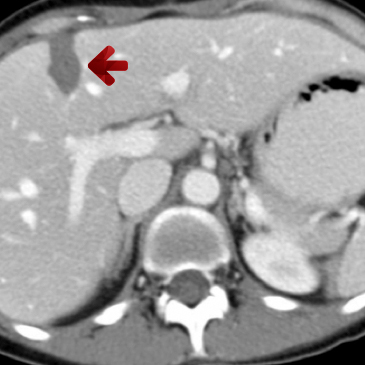
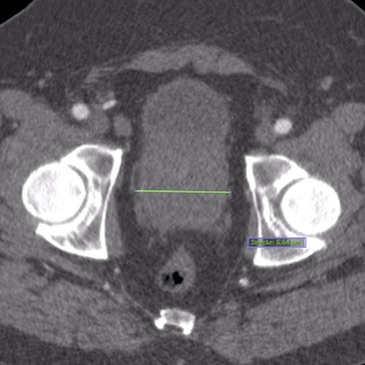
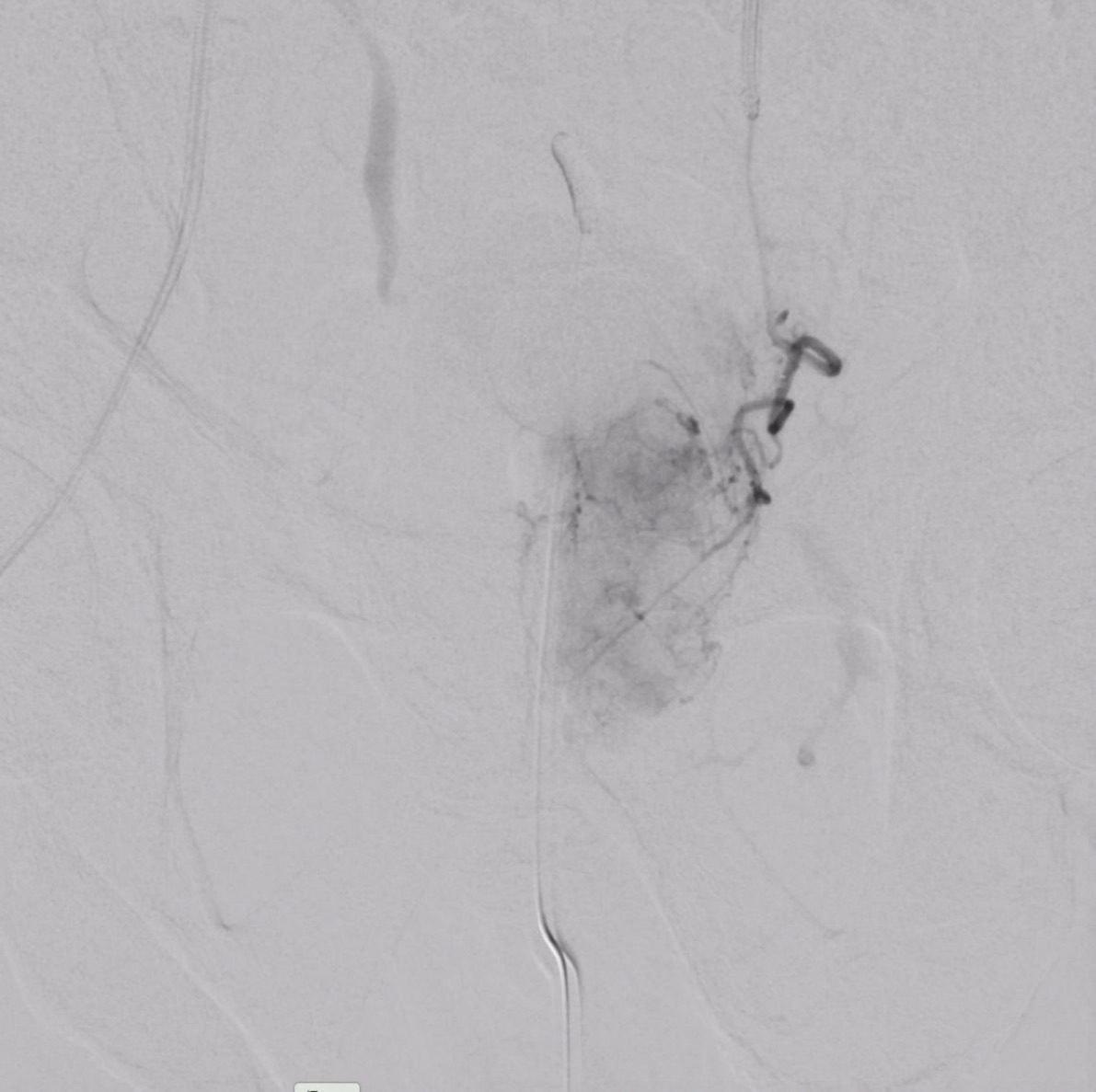
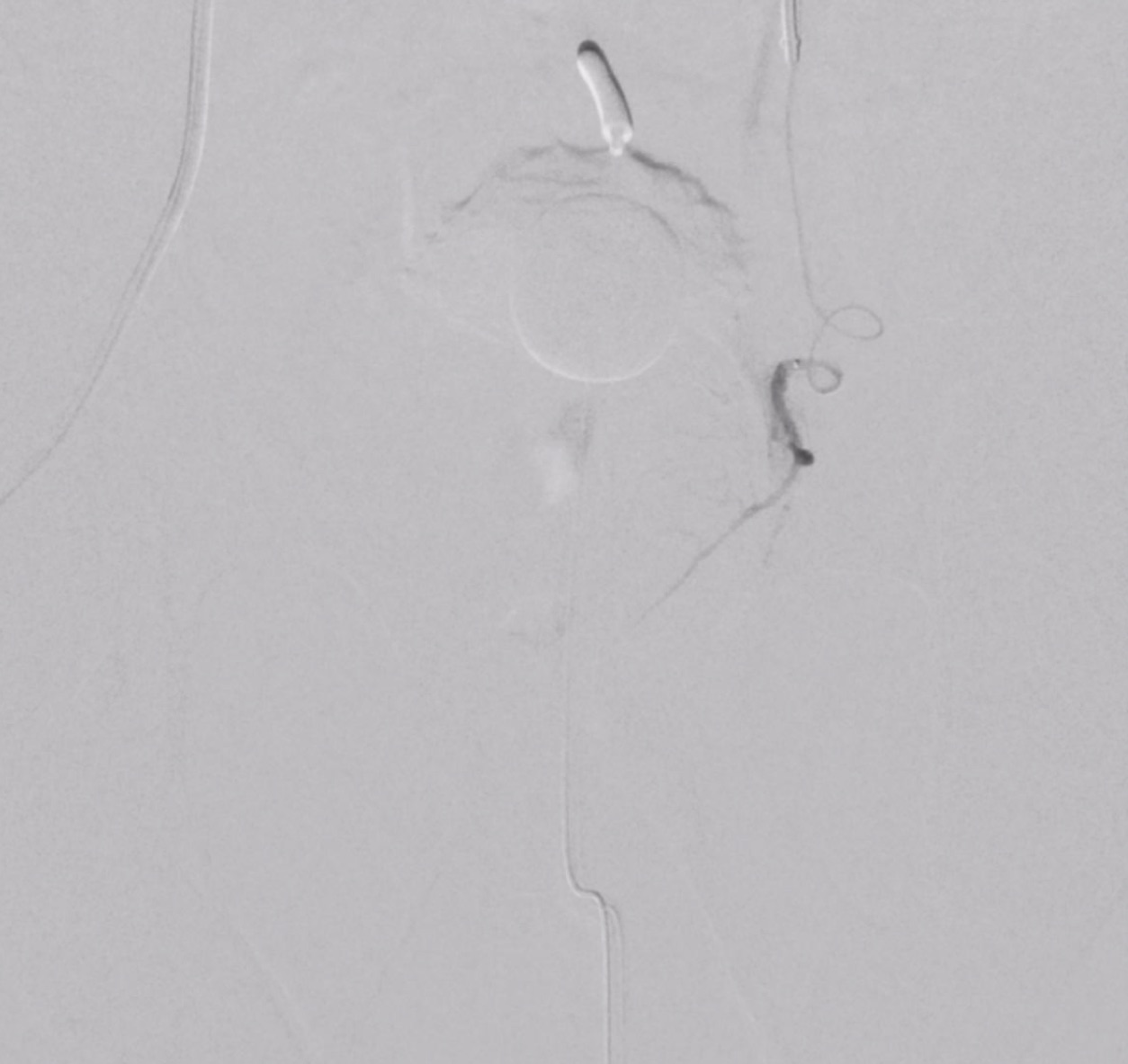
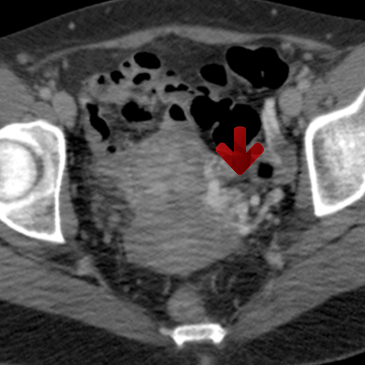
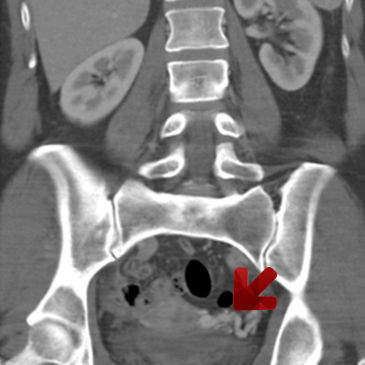
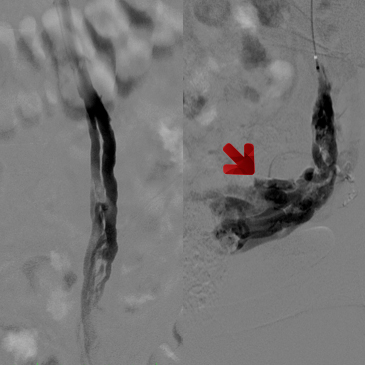
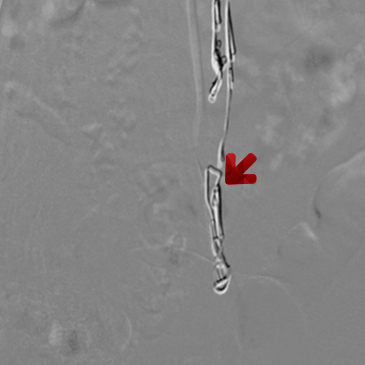
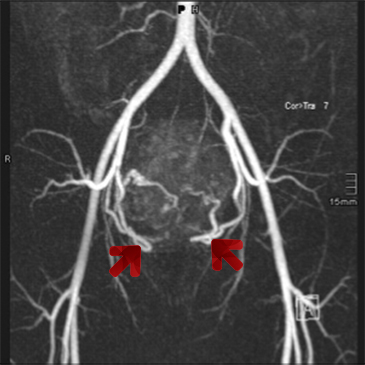
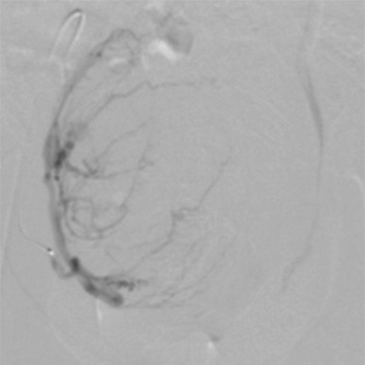
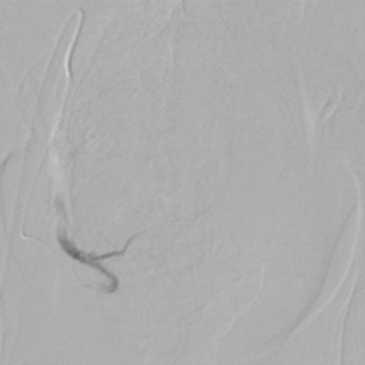
PAOD (=peripheral arterial occlusive disease) as well as occlusive disease in other arterial areas like the visceral, the subclavian, and carotid arteries, are the most common types of vascular diseases that can be treated in a minimally invasive manner.